Breast Reconstruction
- What Is Breast Reconstruction?
- Revisions in Implant Reconstruction
- Direct to Implant Single Stage
- Autologous Tissue Breast Reconstruction
- Autologous and Prosthetic
- DIEP Flap Breast Reconstruction
- Symmetry Matching Procedures
- Pedicled TRAM Flap Breast Reconstruction
- Nipple-Areola Reconstruction
- Free TRAM Flaps
- Nipple-Areola Tattooing
- “Pedicled” TRAM Flap Breast Reconstruction
- Breast Reconstruction Cost
- Prosthetic Breast Reconstruction
- Breast Reconstruction Insurance Coverage
- Expander Implant Exchange and Revisions
Being diagnosed with breast cancer can be the most traumatic event is a woman’s life. Modern treatments of breast cancer include chemotherapy, radiation, and the surgical removal of the breast tumor. In recent years breast surgeons have developed newer procedures that remove the breast tumor but preserve as much of the remaining breast tissue as possible. Many women now have the choice to under lumpectomy and radiation or total mastectomy. For some woman the only option may be total mastectomy.
What Is Breast Reconstruction?
Breast reconstruction is designed to rebuild the breast, typically following cancer treatment, to restore the shape of the natural breast. Depending of the size, location, and severity of the breast defect, women have several options for reconstruction. For women who undergo a lumpectomy, a local skin or muscle flap may be all that is needed to repair smaller defects. For those who require a total mastectomy, reconstruction of the entire breast can be accomplished with prosthetic implants or autologous tissue transfer.
Depending of the size, location, and severity of the breast defect, women have several options for reconstruction. For women who undergo a lumpectomy, a local skin or muscle flap may be all that is needed to repair smaller defects. For those who require a total mastectomy, reconstruction of the entire breast can be accomplished with prosthetic implants or autologous tissue transfer.
As recently as 30 years ago, the options for breast reconstruction were limited. The procedures from that area typically yielded results that were unnatural and gave a less than cosmetically pleasing result. Research and innovation over the last several decades have enabled plastic surgeons to provide their patients with a much more sophisticated range of options. Whether a woman undergoes a unilateral or bilateral procedure, a cosmetically pleasing, natural breast reconstruction may be possible with modern techniques.
I required bilateral mastectomies because of breast cancer. Dr. Z’s caring, guidance, and advice gave me results I never dreamed of! I am happier now with my body (at 55) than I was in my 30’s! I am SO glad I listened and took his advice. His concern and expertise are unmatched!
elizabeth chapman
June 11, 2012
Breast Reconstruction is a vast, complex field with dozens of procedures and possible outcomes. During your initial consultation with our breast surgeon, Dr. Neil J. Zemmel, you will learn about the entire range of options. Our surgeon will perform a complete history and physical to determine your medical and physiological readiness for surgery. Your surgeon will also examine and measure your breasts to determine what procedures will give you the most cosmetically pleasing result.
In general there are three categories of breast reconstruction procedures:
- Autologous Tissue Reconstruction: This refers to using one’s own tissue to recreate the breast.
- Prosthetic Breast Reconstruction: This refers to using tissue expanders and permanent implants to recreate the breast
- Autologous Tissue with Prosthetic Reconstruction: This refers to a combination of the above two techniques to accomplish breast reconstruction
Direct To Implant Single Stage Breast Reconstruction
Traditionally, breast reconstruction has been performed in two stages. The first operation is when the mastectomy is carried out, which leaves the breast with shapeless skin, allowing for gradual expansion over several months. The second operation is typically when a permanent breast implant is placed, finalizing the reconstruction process. However, with the many advancements in the field of breast reconstruction, Dr. Zemmel is pleased to offer a newer technique that requires only one operation. With direct to implant single stage reconstruction, the patient receives the permanent implant at the same time as their mastectomy. This eliminates the need for a tissue expander, though patients have the option to alter their results at a later time. Should they choose to do so, saline solution can be added or removed from the implant via an injection to achieve their ideal size. They can also opt to replace their saline implant with a silicone gel implant.
A benefit of direct to implant single stage reconstruction is that the nipple and areola can often be spared, as long as cancerous tissue is not directly beneath. The technique has proven to work beautifully for those who have small tumors, as well as for women who are considering a preventive mastectomy (those who carry the BRCA gene). Patients typically experience a shorter surgery and recovery period overall, since only one surgery is needed.
During your initial consultation, your surgeon will determine if single stage breast reconstruction is right for you, upon assessing your medical history and discussing with you what you hope to achieve.
Autologous Tissue Breast Reconstruction
 This family of procedures refers to using the patient’s own tissues to reconstruct the breast. Tissues are typically taken from the abdomen, back, or buttocks. The primary advantage of using one’s own tissue is that this tissue will heal and grow with the patient. Unlike with implant reconstruction, there is no future maintenance required. Implant reconstruction sometimes requires replacement of the implants in the event of a rupture or deflation. Tissue reconstructions look and feel more natural. For a one-sided reconstruction, it is easier to obtain better symmetry with a tissue reconstruction.
This family of procedures refers to using the patient’s own tissues to reconstruct the breast. Tissues are typically taken from the abdomen, back, or buttocks. The primary advantage of using one’s own tissue is that this tissue will heal and grow with the patient. Unlike with implant reconstruction, there is no future maintenance required. Implant reconstruction sometimes requires replacement of the implants in the event of a rupture or deflation. Tissue reconstructions look and feel more natural. For a one-sided reconstruction, it is easier to obtain better symmetry with a tissue reconstruction.
The main disadvantage of an autologous tissue reconstruction is that tissue must be harvested and transplanted from an otherwise healthy part of the body. This creates a donor site, which can be rarely subject to complications. For pedicle TRAM flaps, that can result in weakness of the abdominal wall, hernias, and scarring.
If someone told me after surgery I would be feeling this well, I would not have believed them. Dr. Zemmel has exceeded my expectations.
In recent years, there have been dramatic technical advances in autologous breast reconstruction, which is considered by many to be the “gold standard” of breast reconstruction. Advances in microvascular surgery, including “muscle-sparing” techniques and “DIEP perforator flaps”, have made it possible to transfer the necessary tissue with minimal trauma to the donor site. This has resulted in dramatically reduced donor site problems without compromising the outcome of the breast reconstruction. Furthermore, these technological advances have made the option of autologous breast reconstruction a reality for patients who previously were not considered good candidates.
DIEP Flap Reconstruction
The Deep Inferior Epigastric Artery Perforator (DIEP) Flap is one of the most common breast reconstruction techniques performed by Dr. Zemmel. During the operation, they harvest skin and fat tissue from the lower abdomen (similar to a tummy tuck) while sparing the abdominal muscle. This flap is carefully disconnected from its blood supply and then reattached to the blood supply in the chest to form the reconstructed breast. Since the rectus muscle is not removed, patients tend to experience a faster recovery with less pain. This also eliminates the potential of developing specific complications like a hernia or resulting muscle weakness.
A major advantage to undergoing breast reconstruction with the DIEP Flap technique is results tend to look and feel like the natural breast. Additionally, patients can achieve a slimmer tummy area in the same procedure.
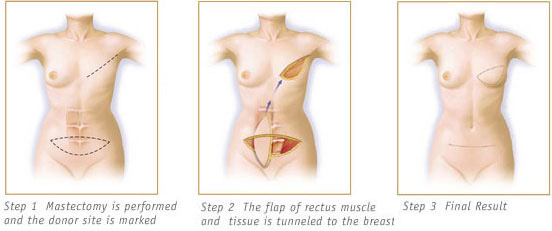
Pedicled TRAM Flaps
 The first successful method of breast reconstruction was the pedicled transverse rectus abdominis myocutaneous (TRAM) flap. This procedure is the most commonly performed tissue reconstruction in the US. In this operation, a wide ellipse of skin and fatty tissue is transplanted from the lower abdomen to recreate the breast. Blood flow must be brought into the tissue so the tissue is left attached to the rectus muscle. The rectus abdominis muscle is taken from the abdominal wall and tunneled underneath the skin of the chest and into the breast. The muscle serves as a conduit for blood flow in and out of the new tissue. Without it the tissue will not survive. The flap gets its blood supply from the superior epigastric artery and vein, which remain attached. Dr. Zemmel closes the donor site with sutures primarily, but also reinforces the abdominal wall with a synthetic mesh typically used in hernia repairs. The flap is then shaped to form a facsimile of a breast.
The first successful method of breast reconstruction was the pedicled transverse rectus abdominis myocutaneous (TRAM) flap. This procedure is the most commonly performed tissue reconstruction in the US. In this operation, a wide ellipse of skin and fatty tissue is transplanted from the lower abdomen to recreate the breast. Blood flow must be brought into the tissue so the tissue is left attached to the rectus muscle. The rectus abdominis muscle is taken from the abdominal wall and tunneled underneath the skin of the chest and into the breast. The muscle serves as a conduit for blood flow in and out of the new tissue. Without it the tissue will not survive. The flap gets its blood supply from the superior epigastric artery and vein, which remain attached. Dr. Zemmel closes the donor site with sutures primarily, but also reinforces the abdominal wall with a synthetic mesh typically used in hernia repairs. The flap is then shaped to form a facsimile of a breast.
The pedicled TRAM flap is capable of achieving very good results and was a tremendous advance in the art of breast reconstruction. For certain patients, it still remains the technique of choice. For some patients, however, (especially those who are obese or who smoke) the blood supply of the pedicled TRAM flap can be insufficient, leading to partial flap loss and poor aesthetic results.
Free TRAM Flaps
Blood flow to a TRAM flap is improved if it is based on the deep inferior epigastric vessels. In this procedure, called the free TRAM flap, these blood vessels are divided and then reattached using microsurgical techniques to recipient vessels in the chest wall or in the armpit. The free TRAM flap has two main advantages over the conventional, pedicled TRAM flap. First, the blood supply is more direct so blood flow is stronger and less likely to cause partial flap loss or fat necrosis. Secondly, only a small part of the rectus abdominis muscle needs be harvested with flap so there is less postoperative pain and abdominal wall weakness. Patients recover from breast reconstruction surgery more quickly and the aesthetic results tend to be better. The main disadvantage of the free TRAM flap is its total reliance on the successful connection or anastomosis of the blood vessels to maintain survival of the flap. If the connection becomes obstructed and blood does not reach the flap, the tissue will die and the breast reconstruction will fail. In experienced hands, the failure rate is less than 2 percent. Failure is even less common in patients who are not obese. Free TRAM flaps require a much longer operative time due to the microvascular reconnection of the blood vessels. Free TRAM flaps yield excellent cosmetic results because of the improved blood flow and ease of shaping the breast flap. Free TRAM flaps also do not require harvesting of the rectus muscle of the abdomen. This significantly reduces the trauma and morbidity to the abdomen wall, reducing the risk of abdominal wall weakness and hernia formation.
“Pedicled” TRAM Flap Breast Reconstruction
In recent years, there have been dramatic technical advances in autologous breast reconstruction, which is considered by many to be the “gold standard” of breast reconstruction. Advances in microvascular surgery, including “muscle-sparing” techniques and “DIEP perforator flaps”, have made it possible to transfer the necessary tissue with minimal trauma to the donor site. This has resulted in dramatically reduced donor site problems without compromising the outcome of the breast reconstruction. Furthermore, these technological advances have made the option of autologous breast reconstruction a reality for patients who previously were not considered good candidates.
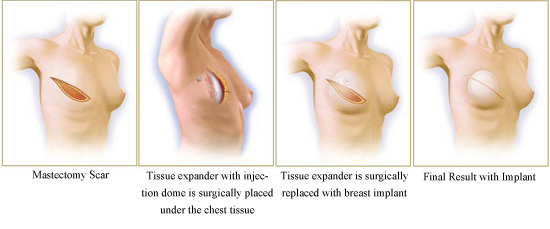
Prosthetic Breast Reconstruction
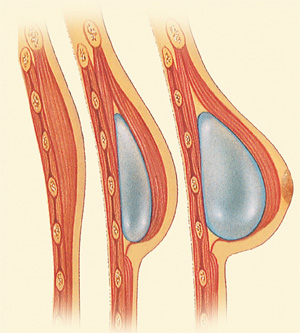 The second option for breast reconstruction, called prosthetic breast reconstruction, uses implants to reconstruct the breast, similar to those used in cosmetic breast augmentation. Unlike a breast augmentation, there is little remaining tissue to cover the implant and a new pocket for the implant must be created. A tissue expander must be inserted into the mastectomy site prior to the insertion of the implant to make a pocket where the implant will ultimately lie. Prosthetic breast reconstruction techniques spare the patient the loss of donor site tissue as well as donor site scarring. Once the tissue expander has healed 2 weeks after surgery, expansion begins. Patients return to the office each week and receive and injection of saline into the expander. This sequentially inflates the expander and stretches the overlying skin. After expansion is completed the patient rests for approximately 3 months to let the tissues come to equilibrium. Patients then return to the operating room and the second stage is completed. This consists of exchange of the tissue expander for a permanent saline or silicone implant. Modifications to the overall breast shape also occur at this stage. Nipple areola reconstruction is performed 3 months after the second stage. The prosthetic breast reconstruction procedures take less time to perform and the hospital stay is generally shorter. However, prosthetic breast reconstructions is a multi-stage procedure performed over 6 to 12 months. A minimum of 2 stages are required. The permanent implant will likely require maintenance in the future.
The second option for breast reconstruction, called prosthetic breast reconstruction, uses implants to reconstruct the breast, similar to those used in cosmetic breast augmentation. Unlike a breast augmentation, there is little remaining tissue to cover the implant and a new pocket for the implant must be created. A tissue expander must be inserted into the mastectomy site prior to the insertion of the implant to make a pocket where the implant will ultimately lie. Prosthetic breast reconstruction techniques spare the patient the loss of donor site tissue as well as donor site scarring. Once the tissue expander has healed 2 weeks after surgery, expansion begins. Patients return to the office each week and receive and injection of saline into the expander. This sequentially inflates the expander and stretches the overlying skin. After expansion is completed the patient rests for approximately 3 months to let the tissues come to equilibrium. Patients then return to the operating room and the second stage is completed. This consists of exchange of the tissue expander for a permanent saline or silicone implant. Modifications to the overall breast shape also occur at this stage. Nipple areola reconstruction is performed 3 months after the second stage. The prosthetic breast reconstruction procedures take less time to perform and the hospital stay is generally shorter. However, prosthetic breast reconstructions is a multi-stage procedure performed over 6 to 12 months. A minimum of 2 stages are required. The permanent implant will likely require maintenance in the future.
Dr Zemmel took something very bad and made it a very good experience for me.
Breast Reconstruction Using Tissue Expanders
 Breast Reconstruction with Prosthetic Implant and “Alloderm sling” Second Stage Prosthetic Breast Reconstruction
Breast Reconstruction with Prosthetic Implant and “Alloderm sling” Second Stage Prosthetic Breast Reconstruction
The second stage of prosthetic breast reconstruction involves removal of the temporary tissue expander and placement of a permanent breast implant. The permanent implant may consist of a saline or silicone depending on the patient’s preference. Our surgeon recommends using silicone implants for reconstruction as this type of implant gives a more natural feel and texture than saline in the setting of reconstruction. Oftentimes the breast pocket may need additional shaping. This may entail raising or lowering of the inframammary fold or expanding or narrowing the width of the breast to reposition the implant. Because the mastectomy has removed the patient’s native breast tissue, the remaining overlying skin may be thin, and implant rippling may be visible. Dr. Zemmel occasionally reinforces the tissue with an acellular dermal matrix (Flex HD or Alloderm). This provides additional tissue thickness to help camouflage any visible parts of the implant. The original mastectomy incision is used so no new incisions are created. Usually no drains are required. This surgery typically has a shorter operative time and quicker recovery. It is usually performed as an outpatient.
Placement of the Permanent Implant Following Tissue Expander Reconstruction
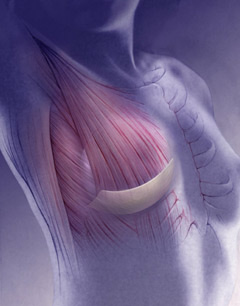
Autologous and Prosthetic Breast Reconstruction
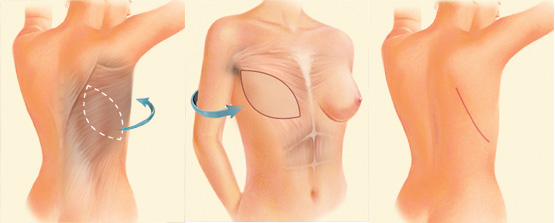
The third option for breast reconstruction is a combination of prosthetic and tissue reconstruction. This option involves the transfer of the patient’s own tissues in combination with the insertion of an implant. This option has both the advantages and disadvantages of the autologous and prosthetic breast reconstruction techniques. However, because expanders are not usually required for these techniques, it is better tolerated by many patients than standard prosthetic breast reconstruction. The most common flap used is called a latissimus dorsi muscle flap. The flap harvests the muscle and skin of the back and tunnels the tissue beneath the skin. Because this flap does not contain sufficient volume, an implant is required. In recent years, there have been dramatic technical advances in autologous breast reconstruction, which is considered by many to be the “gold standard” of breast reconstruction. Advances in microvascular surgery, including “muscle–sparing” techniques and “DIEP perforator flaps”, have made it possible to transfer the necessary tissue with minimal trauma to the donor site. This has resulted in dramatically reduced donor site problems without compromising the outcome of the breast reconstruction. Furthermore, these technological advances have made the option of autologous breast reconstruction a reality for patients who previously were not considered good candidates.
Symmetry Matching Procedures for Breast Reconstruction
Women who undergo a unilateral (one sided) breast reconstruction may require a procedure on the non-reconstructed side to improve symmetry. Depending on the patient’s goals and desires, breast augmentation, breast reduction, or breast lifting may be necessary. These procedure are essentially identical to those performed for cosmetic reasons. For patients undergoing prosthetic breast reconstruction, the symmetry matching procedures are performed during the second stage reconstruction when the tissue expander is exchanged for a permanent implant. Patients undergoing autologous breast reconstruction may require a second surgery to achieve the final breast contour and to symmetry match the other breast. Often times, the nipple areola is reconstructed at this stage. During this stage, your surgeon will have the opportunity to address any issues of the new breast volume in order to improve the cosmesis of the initial reconstruction. This operation is generally performed after the initial swelling from the first surgery has resolved allowing the breast time to heal. If the patient has chemotherapy after the first stage of reconstruction, she can usually have the second surgery performed about one month after completing her treatments. If a patient is undergoing radiation therapy then the second stage is performed 4 to 6 months after the last radiation treatment. The most common revisions in flap reconstruction are corrections of flap volume or contour abnormalities. If the flap is too large, it can be corrected with liposuction or excision of skin and fatty tissue directly. If there is a depression of the soft tissue it may be possible to correct this with fat injections. In this procedure, fat is taken (usually from the abdomen) with liposuction, and is then injected into the soft tissue of the reconstructed breast. Fat injections are not entirely predictable, and it is impossible to predict how much fat will “take” or be accepted by the body. It is not unusual to need more than one procedure to achieve the desired final outcome. The fat that does survive should last forever.
Nipple-Areola Reconstruction
Creating the nipple areola is the final component to making your breast reconstruction complete. Nipple reconstruction is usually performed only after the breast shaping has been completed. Dr. Zemmel usually performs nipple reconstruction 2 to 3 months after the final breast shaping procedure. This allows the breasts to settle into their final form. There is no one absolute best method of nipple reconstruction for all patients. Some patients are comfortable without having a nipple, as they do not wish to undergo any further surgery. Others may choose to forgo nipple reconstruction and have the areola tattooed. This allows color pigmentation to simulate the areola without the projecting portion of an actual nipple. Still, the reconstruction of the nipple areola helps to put the finishing touches on the new breast after a yearlong journey in reconstruction. The most important part of nipple reconstruction is selecting the proper nipple location. Ideally, the nipple should be centered on the new breast mound and its most projecting part. Dr. Zemmel uses modern techniques to achieve nipple reconstruction. He uses local flaps of skin and fat to create a small projecting cylinder of tissue. This technique does not require grafting of skin or labia tissue. Nipple reconstruction is performed in the office under local anesthesia or the outpatient surgery center under light sedation. All nipple reconstructions lose some projection over time as part of the normal wound healing process. Dr. Zemmel will therefore initially create the nipple larger than the desired size in order to compensate for the volume loss. The risk of wound complications in nipple reconstruction is very low in patients with no history of prior radiation, but common in the radiated breast. In the case of failed nipple reconstruction, it may be necessary to revise the reconstruction with another local skin flap. Sometimes, the use of dermis or fat grafts, and fillers may be necessary to improve nipple projection. Alloderm has also been utilized by some surgeons at the time of nipple reconstruction to maximize projection and correct flattening.
Nipple-Areola Tattooing
Tattooing of the areola is the fourth and final component of breast reconstruction. Dr. Zemmel performs this procedure in the office under local anesthesia. If you have a unilateral reconstruction, you will pick and match the pigment color to your native areola. If you have a bilateral reconstruction then you will pick a pigment to closely match your original coloration. Tattooing is relatively non invasive and takes only 15 to 30 minutes to complete. Dr. Zemmel believes creation of a reconstructed nipple and tattooed areola contributes significantly to your overall reconstruction. It can be view as the “finishing touches” on your new breast. Patients are counseled to undergo nipple areola reconstruction whenever possible.
How Much Does Breast Reconstruction Cost?
The cost of breast reconstruction surgery will greatly vary based on the specifics of your treatment plan. Factors such as whether you are receiving a prosthetic or autologous reconstruction, undergoing an immediate or delayed procedure, and the specific technique used to perform your surgery will all impact your total cost. The only way to determine how much your breast reconstruction will cost is to consult with a qualified plastic surgeon to learn about your options. Once you have met with one of our experienced reconstructive surgeons, our staff will provide you with a detailed quote for the fees associated with your procedure. Since all insurance providers that cover mastectomies are legally required to offer coverage for breast reconstruction after cancer, your procedure should be at least partially covered.
Is Breast Reconstruction Covered by Insurance?
The Women’s Health and Cancer Rights Act of 1998 made it mandatory for all group health plans that pay for mastectomies to also cover breast prostheses and reconstructive surgery. Medicare also pays for breast reconstruction, but Medicaid varies on a state-by-state basis. Sponsored plans from churches or the government are not required to cover breast reconstruction after cancer, though they may offer coverage depending on the plan.
To confirm your insurance coverage for breast reconstruction, it is best to contact your provider to learn about the details of your plan. Our knowledgeable staff can also help you navigate your insurance benefits to ensure you receive the most coverage possible. The amount your insurance will cover may ultimately influence which type of reconstruction you move forward with. Keep in mind that your deductible and copays are still out-of-pocket expenses, and this will contribute to your final breast reconstruction cost.





